From Bubonic Plague to Covid-19

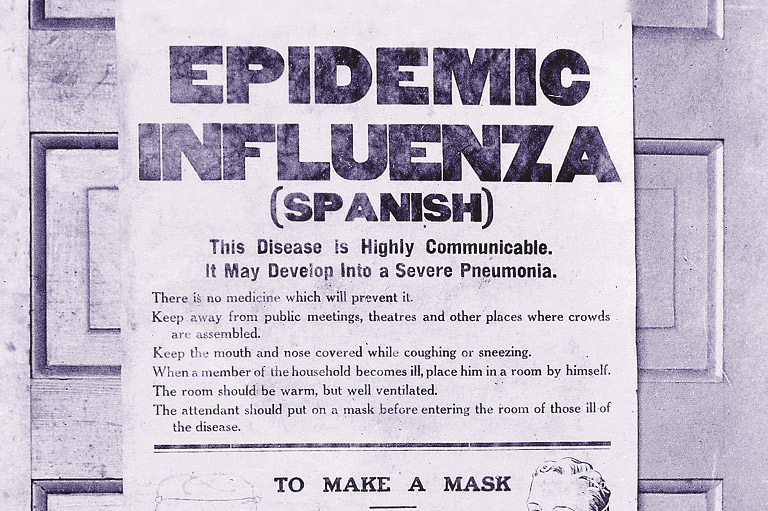
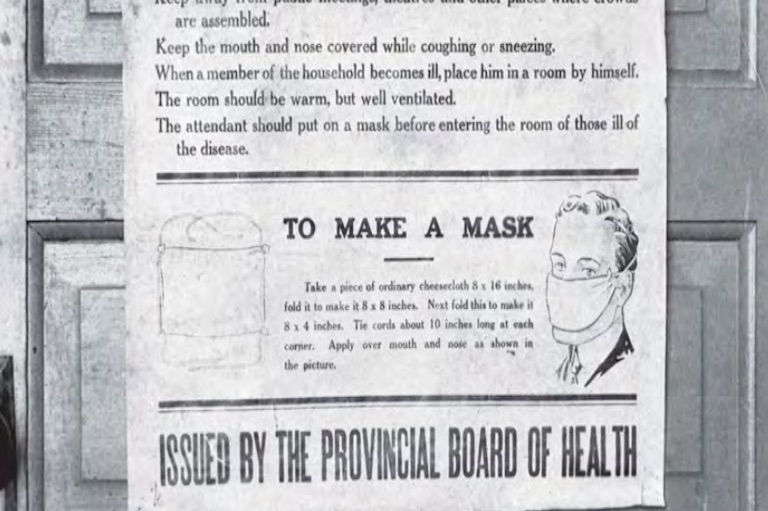
Long before phrases like “social distancing,” “self-isolation” and “flattening the curve” became the linguistic touchstones of the COVID-19 pandemic of early 2020, Canadians had gradually become accustomed to another form of public health language: friendly but insistent public service announcements about the importance of getting an influenza vaccine shot each year, starting some time in the late fall. Health agencies placed ads in bus shelters, newspapers and websites, while drug store chains in some regions moved to offer free inoculations.
These notices encouraged Canadians to take steps to fortify themselves against an infectious disease that can, depending on the year and severity, be merely unpleasant, debilitating and occasionally deadly. Public response has grown over time but influenza immunization rates among Canadian adults under 65 remain less than 40% of the population.1
In the aftermath of the COVID-19 outbreak, however, it seems safe to predict that public health authorities promoting this preventative against influenza, and perhaps, one day, COVID-19, will be dealing with a more receptive audience.
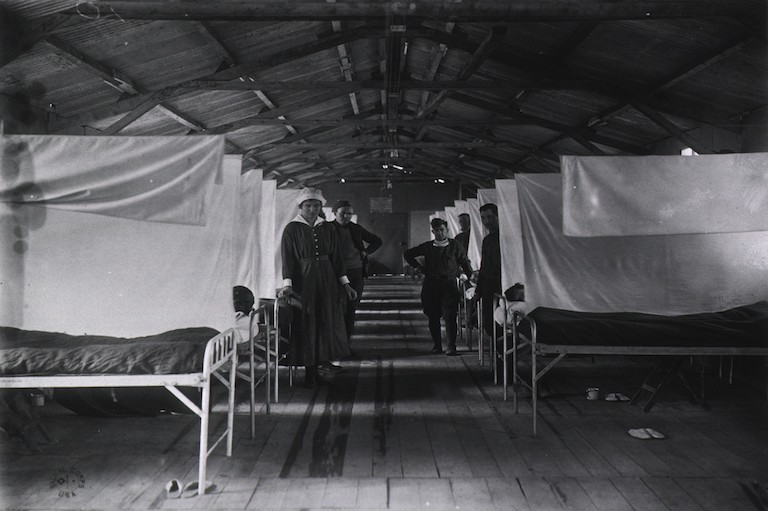
A century ago, after the 1918-1919 “Spanish” influenza pandemic, few Canadians had to be reminded about how deadly a respiratory viral infection could be. Estimates vary, but 50 million to 100 million people worldwide perished in the most devastating pandemic in history – an event that, strangely, has largely receded from memory.
Today, reasonably well-informed people would know that each new wave of influenza originates from Asia and spreads across the globe in predictable patterns. They may also be aware that some strains – H1N1 or Avian flu – can be difficult to treat, while other variants can fuel global pandemics, as has happened not only in 1918, but also in 1957, 1968 and 2019.
Older people will also remember the polio epidemics that worsened across Canada from the late 1920s through the late 1950s during the years before polio vaccines were widely available. “The Crippler” left in its wake close to 50,000 children, as well as adults, with varying degrees of muscle weakness and paralysis, and over 4,100 dead after the poliovirus seriously weakened or paralyzed the muscles that controlled breathing, despite the support of the “iron lung.”2
During the 1980s and 1990s, HIV -- which attacks the immune system and is passed by sexual contact, blood transfusions and intravenous drug use -- spread rapidly around the world. Acquired Immune Deficiency Syndrome (AIDS) was lethal until the development of treatment regimes, public education campaigns and otherprevention measures.
In 2003, thousands of people fell ill, and many died, during an especially severe outbreak in Toronto that seemed to target hospitals and health care workers. This was “SARS” (Severe Acute Respiratory Syndrome), a pneumonia-like infection caused by a novel coronavirus (similar to COVID-19) that began in China and was imported into Canada.3
Meanwhile, certain sub-populations, like homeless shelter users, as well as Indigenous communities, especially Inuit, have experienced tuberculosis (TB) outbreaks, although public health authorities have taken steps to contain the spread among vulnerable individuals.4
And in recent years, measles has made a dramatic come-back in many parts of the world and some Canadian cities due to growing numbers of parents who refuse to inoculate their infants out of a concern, stoked on social media but unfounded scientifically, about a link between measles vaccines and autism.
But until the COVID-19 pandemic, it would be fair to say that contemporary urbanized societies were no longer especially preoccupied with the threat of widespread infectious disease outbreaks that ravaged entire communities in previous eras. While this prevailing sense of security is rooted in genuine confidence in public health protections and medical science, it also reveals a kind of social complacency and amnesia about the damage that infectious diseases, whether caused by familiar or novel viruses and bacteria, are capable of inflicting.
Among all of these earlier examples, the “Spanish” influenza pandemic was unique in its intensity and extent. Its story also offers 21st century Canadians, with our modern health care and state-of-the-art medicine, powerful insights into the impact and aftermath of the COVID-19 pandemic.
By learning and remembering and honouring that history, we are also showing respect for the power of nature to inflict suffering and death. For the bulk of recorded history, human beings have lived with the threat of sudden death or infirmity at the hands of diseases they didn’t understand. We understand much more today, but our well-being still depends not just on science, but also on a broad and deep understanding of the stories of past tragedies.
During the Middle Ages in much of Europe and through the 19th century, urban populations in much of Europe and Asia were regularly decimated by pandemics associated with rat infestations, contaminated water and crowded conditions. Bubonic plague was one of the most deadly diseases, transmitted by fleas and parasites. According to the World Health Organization, the bubonic plague – also known as “The Black Death” – killed about 50 million people in 14th century Europe and continued to circulate for centuries.
The plague still exists, with several thousand people infected each year worldwide, although the disease is now easily treated with antibiotics.5 For generations, rats were seen as the vector of infection, but recent research suggests that the plague spread through the transmission of human parasites.6
Later on, the conditions of urban life as well as mass migration became key factors driving the rapid spread of highly infectious and deadly diseases such as smallpox, typhus and cholera, which thrived in cities where water supplies, like wells or rivers, were polluted with human waste (feces). Successive epidemics of cholera, which causes extreme diarrhea and can bring on death from dehydration within hours of exposure7, swept through Europe and spread to North America on ships filled with migrants from Britain.
In Canada, cholera arrived in the 1830s8 and triggered health emergencies in cities like Montreal and Toronto, prompting unprepared authorities to establish the earliest public health boards. Local officials hastily buried the dead in mass graves to prevent further infection.9
At the time, no one knew how cholera, or indeed most infectious diseases, spread from one individual to another. Scientists hadn’t yet discovered bacteria or viruses (“germs”), the microscope hadn’t been invented and the concept of vaccination was in its infancy.
“Vaccination” was discovered by Edward Jenner in the 1790s to prevent smallpox using vaccinia virus collected from cows (“vacca” is Latin for cow). In fact, one of the prevailing explanations for disease transmission focused on the concept of “miasma,” or bad or putrid air – an idea that traced back to the ancient Greeks and persisted into the late 19th centuries despite advances in microbiology.10
As a 2010 history of Canadian public health by Christopher Rutty and Susan Sullivan points out, 18th and 19th century colonial governments enacted draconian quarantine laws, but these often failed to be enforced by local officials.11
A turning point in the containment of infectious disease outbreaks occurred during a cholera epidemic in London, England, in 1854. Tens of thousands of Londoners had died of cholera epidemics in 1849 and 1853. Reformers and health officials were focused on addressing disgusting living conditions characterized by over-crowded houses whose basements were literally overflowing with human waste disposal and the widespread use of the Thames as an open sewer.
During a 1854 cholera outbreak, a young physician named John Snow came up with the idea of mapping the addresses of victims in an west-end neighbourhood centred on Broad Street.
When he analyzed his famous “ghost map,” he realized that many of the sick and dead lived close to an outdoor water pump that drew on a well contaminated by a nearby privy. By contrast, people who worked at nearby local breweries tended not to fall ill. Snow’s empirical observations, considered to be among the first breakthroughs of modern epidemiology, prompted local officials to remove the handle on the Broad Street water pump, a turning point in public health policy.12
During the late 19th and early 20th centuries, many public health advocates and governments pushed to implement prevention-oriented improvements geared at limiting the spread of diseases like cholera – modernized sewers and fresh water infrastructure, housing design standards, the development of sanitary burial rules for cemeteries, and eventually, measures such as chlorination, milk pasteurization and regulations governing abattoirs, and the processing and handling of raw meat.
The mass production of vaccines and the advent of large-scale inoculation campaigns shifted the fight against infectious disease and epidemics into the realm of preventative medicine. But vaccination wasn’t immediately accepted as a preventative measure.
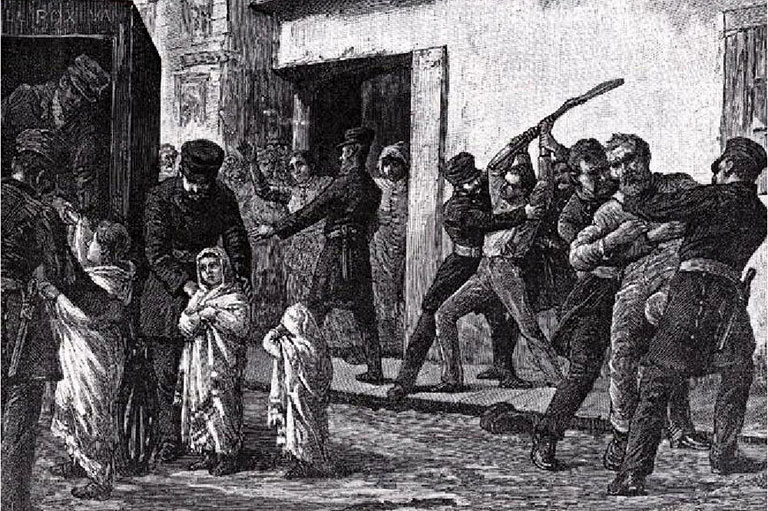
During a devastating smallpox outbreak in Montreal in 1885, provincial and municipal officials made vaccination mandatory. But as historian Michael Bliss explains in his book, “Plague: A History of Smallpox in Montreal,” Protestant (mostly anglophone) communities were far more accepting of the inoculation campaigns than Catholic (mostly francophone) neighbourhoods, and thus experienced far lower rates of disease.13
Despite the controversy, routine vaccinations have become one of the principal prevention measures against a range of infectious diseases. Smallpox was declared eradicated from the globe in 1979, and polio is close to the same goal. Launched in 1988, the global polio eradication initiative has reduced global polio incidence by 99%; only a handful of highly unstable countries continue to see cases today.14
Yet not all infectious diseases that turn into epidemics have been purged as effectively as smallpox and polio. Yemen, for example, has seen a dramatic surge in cholera in recent years – “the largest and fastest-spreading outbreak of the disease in modern history, with a million cases expected by the end of the year and at least 600,000 children likely to be affected,” as The Guardian reported in October, 2017.15
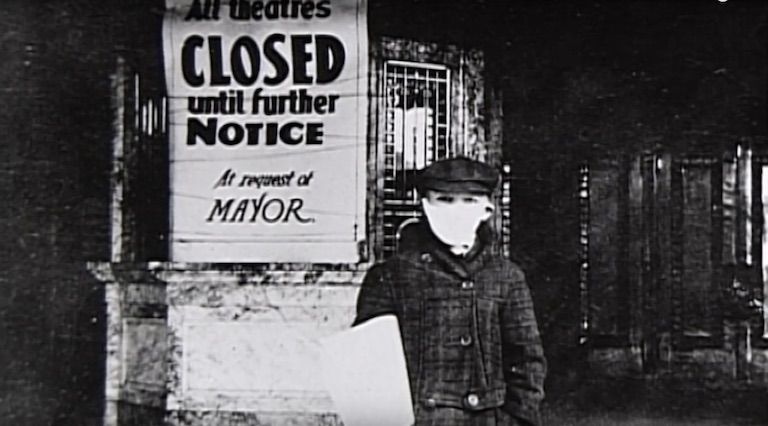
What are the connections between today’s national and global public health practices and the pandemic that ravaged so much of the world in 1918? The answer is complicated in part because so much about the Spanish Influenza pandemic has been forgotten. Yet epidemiologists today understand more about the vectors of infection because they’ve examined how pandemic influenza spread, especially in North America, from troops traveling to and from European battlefields and then between the U.S. and Canada.
Scientists now know how the highly variable molecular structure of the influenza virus can produce limited or deadly infections. We drew on some of these lessons during and after the SARS pandemic, in 2003, although dramatic evidence that’s surfaced during the COVID-19 pandemic -- about critical shortages of medical supplies and equipment -- reveal what can happen when shocking events recede from memory.
There is, in fact, far more to learn from 1918, especially how ordinary people were forced to deal with this disease so close on the heels of a terrible war.
The Defining Moments Canada website provides a wealth of information about the way Canadians were affected by this pandemic. The content includes a range of perspectives on an event that has mostly receded from memory, including scholarship on the evolving public health policy environment, political reaction and scientific explanations for the way this family of diseases spreads.
Most importantly, DMC includes a wide range of entries drawn from primary sources and oral histories which, taken together, will reveal how “Spanish” influenza ravaged military camps, urban/ethnic neighbourhoods, remote rural and Indigenous communities, and even the 1919 Stanley Cup final.
This Centennial project aims to create a virtual hub for digital story-telling that aspires to commemorate and document the influenza pandemic in Canada -- a profoundly transformative event that has, nonetheless, all but slipped from collective memory. The site draws on the innovative student engagement and digital story-telling techniques developed for the Digital Historian Project, an award-winning collaboration between the Upper Grand District School Board and the Dufferin County Museum and Archives.
Our goal is inoculate ourselves from the lethal consequences of collective amnesia – a project that seems exponentially more important today than when this project launched in 2018. We seek to remember not just for its own sake, but to ward off the complacency that can leave our communities vulnerable to, and ravaged by, future epidemics.